The coronavirus has shaken the world and shown the need for innovation in hospitals. However, much emphasis has been put on product and technological innovations such as emergency ventilators and masks, while service innovations involving new ways of providing health care often remain under the radar.
In order to increase the visibility of hidden innovations, a national innovation monitoring and management system is currently under development. Although the use of the tool is still in the early phase of adoption, its deployment in hospitals has enabled identification, sharing and learning among and beyond hospitals.
Trust Saidi, Post Doc, TIK Centre, University of Oslo
Taran M. Thune, Professor, TIK Centre, University of Oslo
Markus Bugge, Professor Associate, TIK Centre, University of Oslo
Service innovations are crucial but hardly recognised
Service innovation plays a crucial role as society’s engine of renewal, and services are particularly important in the public sector (Synder et al., 2016). Moreover, hospitals constitute an important part of the organisations dedicated to the provision of public health services. As such, many hospitals are actively promoting innovation and developing competences in managing, selecting and evaluating innovations.
However, service innovations such as new practices and management techniques are closely related to everyday work and hence hidden and traditionally underestimated. The challenge is that the hiddenness of service innovations renders it difficult to capture them, therefore they can often be both «under-recognized», «under-developed» and «under-diffused».
Ongoing work at the Centre for Technology, Innovation and Culture (TIK), University of Oslo, focuses on how service innovations in Norwegian hospitals can be legitimised, incentivised, monitored and managed to ensure that they are more effectively and systematically identified and diffused.
The project is motivated by the need to capture the kinds and volume of service innovations carried out by most hospitals and hospital staff as stipulated in a «commission document» by the Ministry of Health:
There is a need to assess and develop the existing set of indicators for innovation in the health care sector. Measurement of innovation activity in health care organizations should capture all aspects of innovation, including changes that are the results of process- and service innovations. The indicators should include both commercial and non-commercial innovation activity (Ministry of Health, 2011).
A common innovation monitoring and management tool
The challenges in capturing service innovations are attributed to their very nature. These include intangibility in that they cannot be apprehended by the physical senses, simultaneity as they are concurrently produced and consumed, perishability due to the fact that they are used as offered with no possibility of storage, return, sale or even subsequent use and heterogeneity which emanates from the variability in the quality parameters, since they are transmitted from people to people (Moeller, 2010).
Considering the difficulties linked to capturing service innovations, we attempted to understand the development and implementation of a common innovation monitoring and management tool developed for the Norwegian Ministry of Health. The tool has been implemented in different hospitals across the country as a pilot project on a voluntary basis. It is built on a phase-model, where innovation projects are described in five main phases as shown below:
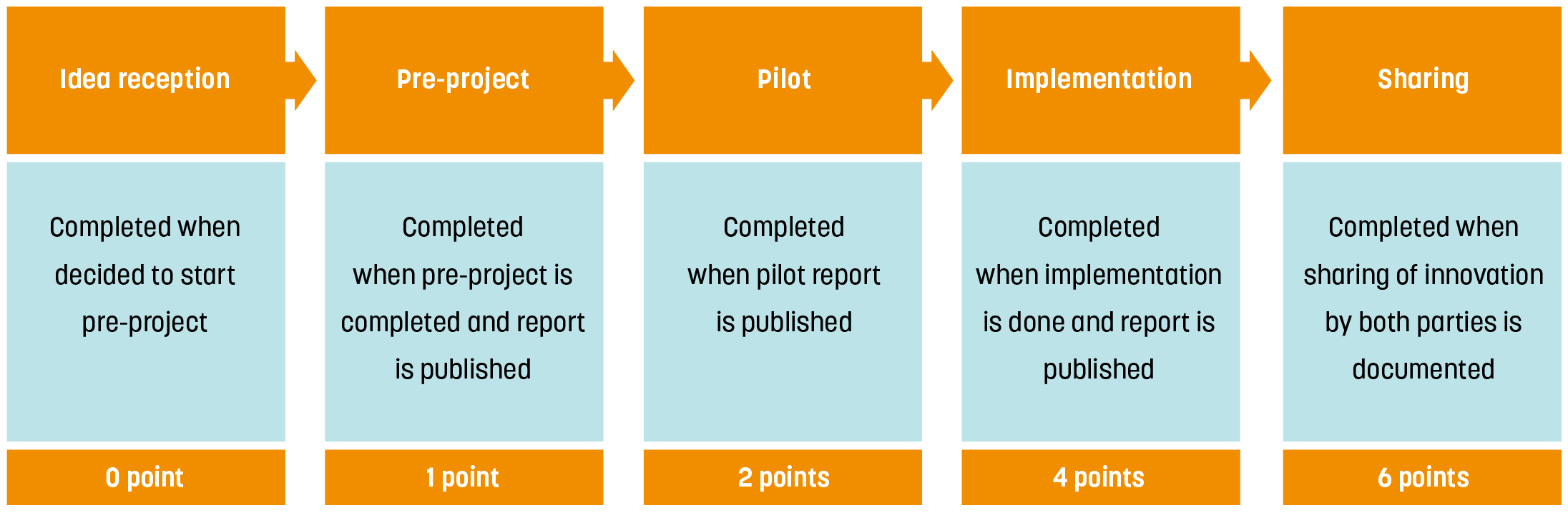
The tool is based on the idea that all kinds of innovations move through similar stages and that decisions (stop-go) need to be taken at important «gates». A project accumulatespoints throughout the process and by allocating the highest number of points at the sharing stage, the system incentivises diffusion of innovation. The points for sharing are given to both the originated project and adopted project.
A tool for mediating, learning and sharing
Since innovation is not a linear process, but rather a dynamic approach which is an output of interactive sequences (Corona- Treviño and Márquez-Aguilar, 2017), the use of the monitoring and management tool serves as a mediating object that brings different hospitals together. As a mediating object, the tool provides a site for collective activity where stakeholders from hospitals generate a shared intention and capability for action.
This has the positive effect of fostering collaborations and facilitating learning-bydoing, using, and interacting. As the tool is anchored on the notion of open innovation involving purposive flow of knowledge with the aim of accelerating both internal and external use, sharing is an indispensable component of its implementation.
This has resulted in hospitals engaging each other by identifying projects of common interests. Instead of «reinventing the wheel», the hospitals have the option of adopting the innovations, which is an effective way of saving resources.
Limited motivation to drive service innovations
Despite the promising results on the use of the tool, there are challenges in scaling up its use in hospitals. The nurses and doctors to whom the tool is targeted to promote sharing of innovations are overwhelmed by their daily work tasks. Despite their interests to work on innovations, they hardly have time, hence there is a need to improve their opportunities to do so.
Moreover, some staff consider innovation to be beyond their scope, yet they do not need to ’invent to innovate’, as incrementalinnovations can also contribute to significant gains in the delivery of services. This may require interventions, such as capacity building and using incentives in different forms to motivate them. As the hidden innovations in hospitals are being captured, there are prospects for measuring them and possibly developing an indicator system for rewarding innovators.
With proper planning, coordination and management of service innovations, it is likely that such innovations can become more visible and acknowledged. It takes time to achieve this, and there may be many steps towards building a culture of innovation. In addition to this new management tool, an innovation culture can also be stimulated through existing incentive structures in the health sector.
In the face of the coronavirus pandemic, there is now an opportunity to highlight the engagement, capacities and capabilities of professional health care staff, and their role in capturing and sharing service innovations in hospitals.
References
– Corona-Treviño, L., & Márquez-Aguilar, C. (2017). Characteristics of service innovation in hospitals: A case study of three Mexican hospitals. In Service business model innovation in healthcare and hospital management (pp. 159-178). Springer, Cham.
– Moeller, S. (2010). Characteristics of services – a new approach uncovers their value. Journal of Services Marketing, 24 (5), 359-368.
– Snyder, H., Witell, L., Gustafsson, A., Fombelle, P., & Kristensson, P. (2016). Identifying categories of service innovation: A review and synthesis of the literature. Journal of Business Research, 69(7), 2401-2408.
Hovedfoto: FatCamera.

